Frequently Asked Questions
Your Guide to Endodontic Treatment
You’re probably reading this because your dentist or endodontist has said you need endodontic treatment. If so, you’re not alone. More than 14 million teeth receive endodontic treatment each year.
By choosing endodontic treatment, you are choosing to keep your natural teeth as a healthy foundation for chewing and biting for years to come.
If you’ve never had endodontic treatment–also known as a “root canal” — or if it has been many years since your last procedure, you may have questions or outdated expectations. Technology has advanced dramatically over even the past several years.
What is an endodontist?
Endodontists are dentists with special training in endodontic procedures; essentially, they are root experts. They only do endodontic procedures in their practices because they are specialists. To become specialists, they complete an additional two or more years of advanced training in endodontics following dental school. They perform routine as well as very complex endodontic procedures, including root canals, root canal retreatments, and endodontic microsurgery. For more information about each of these procedures, please read under Services. Endodontists are also experienced at finding the cause of oral and facial pain that has been difficult to diagnose.
Why choose an endodontist?
- Endodontists are dentists with at least two additional years of advanced specialty education in diagnosis and root canal treatment.
- Because they limit their practices to endodontics, they treat these types of problems every day. They use their special training and experience in treating difficult cases, such as teeth with narrow or blocked canals, or unusual anatomy.
- Endodontists may use advanced technology, such as microscopes, ultrasonics, and digital imaging to perform these special services.
What are the main root canal symptoms patients should be aware of?
There are two main diagnoses that require initial endodontic treatment due to a diseased pulp or root canal system. The first is called irreversible pulpitis, which is when the nerve space is inflamed. The main symptoms for this diagnosis include:
- Lingering pain to cold
- Spontaneous toothache
- Pain to biting or pressure
The second diagnosis that requires endodontic treatment is pulp necrosis, which is when the nerve has died. These teeth usually don’t have pain to cold but instead you’ll notice:
- Spontaneous toothache
- Severe pain to biting or pressure
- Swelling
- An area that drains pus on the gum
Some root canal problems, though, are asymptomatic, so your dentist or endodontist may find the issue on an x-ray or see it clinically—and it may not be related to pain at all.
What is endodontic treatment?
“Endo” is the Greek word for “inside” and “dont” is Greek for “tooth.” Therefore, endodontic treatment treats the inside of the tooth, or the pulp of the tooth.
To understand endodontic treatment, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves, and connective tissue. Its main purpose is to develop the tooth during adolescence.
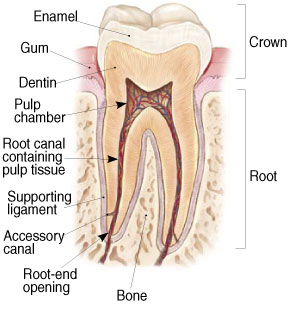
The pulp extends from the crown of the tooth to the tip of the roots where it connects to the tissues surrounding the root. The pulp is important during a tooth’s growth and development. However, once a tooth is fully mature it can survive without the pulp, because the tooth continues to be nourished by the tissues surrounding it.
Why would I need an endodontic treatment?
Endodontic treatment is necessary when the pulp becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, a crack or chip in the tooth, or trauma. Trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
Signs of pulp damage include pain, prolonged sensitivity to heat or cold, discoloration of the tooth, and swelling and tenderness in the nearby gums. Sometimes, there are no symptoms, and the infection or inflammation can only be detected on the x-ray by your dentist or endodontist.
If patients are nervous about getting a root canal, what should they be aware of that may help them relax?
Standard root canal treatment is done thousands of times every single day all over the world—and new technologies in anesthesia and instruments used during a root canal make it a painless experience. Patients should also know that being anxious about a dental procedure is very common, and they are not alone in their feelings.
What can occur if a patient decides to delay having treatment done?
Delaying treatment or deciding on no treatment can lead to:
- Increased pain
- Infection
- Swelling
- Bone loss around the tooth
All of these things can decrease a patient’s ability to heal, so it’s important to not delay treatment if you’re experiencing any symptoms of infection.
How does endodontic treatment save the tooth?
The endodontist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the tooth, then fills and seals the space. Afterwards, you will return to your dentist, who will place a crown or other restoration on the tooth to protect and restore it to full function. After restoration, the tooth continues to function like any other tooth. For a step-by-step explanation of the procedure, please read under Services: Root Canal Treatment.
Can all teeth be treated endodontically?
Most teeth can be treated. Occasionally, a tooth can’t be saved because the root canals are not accessible, the root is severely fractured, the tooth doesn’t have adequate bone support, or the tooth cannot be restored. However, advances in endodontics are making it possible to save teeth that even a few years ago would have been lost. When endodontic treatment is not effective, endodontic surgery may be able to save the tooth.
What are the advantages of a patient keeping his or her natural tooth?
It’s so important to save our natural teeth because that’s the best way to maintain strong chewing function and aesthetics. While it costs less money to extract a tooth than to save it with endodontic treatment, it starts to get much more costly when you consider placing a dental implant. Studies have shown great survival of endodontically treated teeth with less postoperative cost and complications than what occurs with tooth replacement with dental implants.
For a tooth with a favorable prognosis, it’s better to do a root canal, retreatment or apical surgery to preserve it for as long as possible before resorting to extraction and a dental implant.
Will I feel pain during or after the procedure?
Many endodontic procedures are performed to actually relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, patients generally report that they are very comfortable during the procedure. Many even say that getting a root canal is easier than having a crown prepared! While feeling pressure and vibration is normal during a root canal procedure, experiencing pain is NOT normal. If any pain is experienced, Dr. Potter asks that you raise your left hand so she can stop what she is doing and do everything in her power to get you more comfortable.
For the first few days following treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This tenderness is especially prominent with biting on the tooth because the ligament that surrounds your tooth is starting to heal. This discomfort can be relieved with over-the-counter or prescription medications. Follow your endodontist’s instructions carefully.
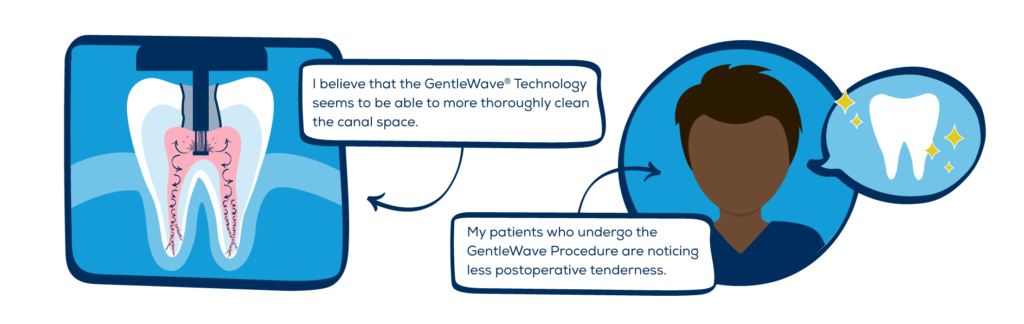
What is the biggest benefit of the GentleWave procedure for patients?
The biggest benefit of the GentleWave Procedure is achieving a cleaner canal system while removing less dentin. We believe that this will ultimately lead to a better success in saving natural teeth—hopefully for a lifetime. Another benefit is that the technology cleans the canals so thoroughly that many patients are experiencing less post-operative pain as compared to traditional root canal treatment.
How much will the procedure cost?
The cost varies depending on how severe the problem is and which tooth is affected. Molars are more difficult to treat and usually cost more. Most dental insurance policies provide coverage for endodontic treatment.
Generally, endodontic treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic treatment and the appropriate restoration. For detailed information on cost, please consult with our office’s financial manager. If cost is a concern, we offer interest-free financing through Care Credit. You can gather more information about this financing at www.CareCredit.com.
For more information, please view our Forms & Policies page.
Will the tooth need any special care or additional treatment?
You should not chew or bite on the treated tooth until you have had it restored by your dentist. In addition to it being sore to biting for the first few days, accidentally biting something hard before you see your dentist can be detrimental to the long-term success of the treatment. The un-restored tooth is susceptible to fracture, so you should see your dentist for a full restoration as soon as possible. Otherwise, you need only practice good oral hygiene, including brushing, flossing, and regular checkups and cleanings.
Most endodontically treated teeth last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic treatment fails to heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this happens, another endodontic procedure can save the tooth.
What causes an endodontically treated tooth to need additional treatment?
New trauma, deep decay, or a loose, cracked, or broken filling can cause new infection in your tooth. In some cases, the endodontist may discover very narrow or curved canals that could not be treated during the initial procedure. For further information about root canal retreatment and endodontic (apical) surgery, please review our Root Canal Retreatment and Endodontic (Apical) Surgery pages.
What are the alternatives to endodontic treatment?
When the pulp of a tooth is damaged, the only alternative to endodontic treatment is extraction of the tooth. To restore chewing function and to prevent adjacent teeth from shifting, the extracted tooth must be replaced with an implant or bridge. This requires surgery or dental procedures on adjacent healthy teeth and can be far more costly and time-consuming than endodontic treatment and restoration of the natural tooth.
No matter how effective modern tooth replacements are–and they can be very effective–nothing is as good as a natural tooth.
Following Endodontic Treatment
Your root canal has now been completed. The canals have been cleaned and sealed. Your body must now have time to repair the tooth and its surrounding area.
It is normal for the tooth to be very sore for the first few days, and it may remain sensitive to biting pressure for up to six weeks. Three Advil (600mg total) or 2 Extra-Strength Tylenol (1000mg total) every 4-6 hours will usually relieve the soreness. If the discomfort is more severe, please let us know so that we may prescribe an appropriate medication. If pain persists or increases, or swelling develops, please contact the office.
Antibiotics are generally not required following root canal therapy. Your doctor will prescribe them when indicated.
Do not chew on the tooth until all tenderness is gone. This will likely be at least 3 days. This will prevent you from bumping the sore tooth and allow it to heal.
Many times after endodontic treatment a temporary filling is placed in your tooth. You should now return to your dentist, who will place the appropriate final restoration. Do not chew on your treated tooth until it has been properly restored by your general dentist. There is a risk of fracturing the tooth.
If it is recommended by your endodontist to check the tooth in 6 months to monitor healing, please call to set up your complimentary recall visit when appropriate.
Direction for Pain Management
For Mild to Moderate Discomfort
Take 600 mg of Ibuprofen (Motrin, Advil, etc.) or 1000mg Acetaminophen (Tylenol) every 4-6 hours.
For Moderate to Severe Pain
For moderate pain, begin with 600 mg Ibuprofen.
Two hours later take 1000mg Tylenol
Two hours after that take another 600 mg Ibuprofen
Continue to alternate 600mg Ibuprofen and 1000mg Tylenol as needed. These two potent anti-inflammatory drugs work synergistically together to fight inflammation and pain.
NEVER exceed any 1 medication sooner than every four (4) hours.
You may discontinue the medication as discomfort decreases.
If you experience any reaction from the medications which appear to be abnormal, stop the medication and call our office. If this does not relieve your pain, please call us, as Dr. Potter may want to prescribe you a stronger medication.
Following Endodontic (Apical) Surgery
Bleeding
A certain amount of bleeding or oozing is to be expected near the sutures. If needed, you can put some pressure with moist gauze on the area for 30 minutes. You can also place a moistened tea bag directly over the surgical site for at least 10 minutes, holding it in place with moderate biting pressure. If bleeding continues, repeat. Do not smoke for 24 hours. Forceful spitting and excessive physical activity tend to increase and prolong bleeding. Resting in a semi-reclining position for the first few hours is highly recommended.
Pain
Take your pain medication as directed by your doctor.
Rinsing
It is likely that Dr. Potter will prescribe a prescription mouth rinse (Chlorhexidine/Peridex) for your surgery. You should rinse twice a day with this for 30 seconds. Do not eat or drink for 30 minutes following your rinse. In addition to this prescription rinse, you may also rinse with warm salt water 4 or 5 times a day for several days (add 1/2 teaspoon of salt to a glass of warm water). After 24 hours you may gently brush your teeth. However, flossing in the area of surgery should be avoided.
Swelling
To help minimize ordinary post-operative selling, apply an ice pack to the face over the area of surgery for a few hours. Place the ice pack on for 5-20 minutes, followed by a 5-20 minute break, and repeat.
Diet
It is important to maintain a good diet and remain well hydrated following your surgery. A liquid to soft-food diet is advisable for the first 2 days. This includes such things as applesauce, soup, pudding, Jell-O, spaghetti, ice cream, malts, etc. You should drink at least 8 glasses of liquid per day.
Unusual Complications
Feel free to contact us if any concerns arise regarding your recovery.
Avoid strenuous activity for the remainder of the day. Smoking and alcohol consumption should be avoided for three days.
For the first 48 hours eat soft foods only and drink lots of fluids. In addition to fruit juices, soups and other soft foods, liquid food supplements are recommended. (Example: SlimFast, Ensure, etc.)
Avoid facial manipulation as much as possible. Do not raise the lip or retract the cheeks to inspect the surgical site as you may dislodge the sutures (stitches).
Swelling and discoloration (bruising) sometimes follows surgery. To minimize this, apply an ice bag alternately 5-20 minutes on, 5-20 minutes off, for a few hours following the surgery.
Take all medications as directed.
You will be advised to return to our office 3-7 days following surgery for a post-op evaluation by Dr. Potter and any necessary suture removal.
Location & Contact
665 Camino de los Mares, Suite 204
San Clemente, CA 92673
Map & Directions
Phone: (949) 661-9680
Fax: (949) 661-4872
Email: Contact Us
Office Hours
Mon – Fri: 8am – 5pm